What is MRKH Syndrome?

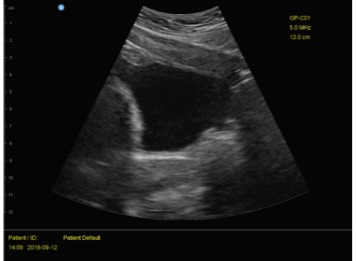
Mayer-Rokitansky-Küster-Hauser Syndrome, abbreviated MRKH Syndrome, is a disease that affects 1 in every 4000-5000 female births,1,2 and causes these babies to be born without certain reproductive organs. This occurs during development because the embryological structures that go on to form these organs are either absent or fail to develop.1 Therefore, the baby is born with no uterus, cervix, or upper part of the vagina.1 Other embryological structures develop normally, such as that which becomes the ovaries, allowing external genitalia to have a normal appearance and secondary sex characteristics to be expressed.1 It is still unclear as to why this happens, but several etiologies are being considered including monogenic, oligogenic, polygenic, multifactorial, and environmental factors.1 The first sign of MRKH Syndrome is usually primary amenorrhea (absence of menses),1 which will become evident at 15-21 years of age.2 Those with MRKH syndrome will also present with a short, blind ending vagina (0-3cm), however female karyotype and hormone levels are all normal.1
Associated Symptoms
MRKH syndrome is often associated with psychological and/or psychosexual issues.3 Mental health support is extremely important upon diagnosis of MRKH syndrome and throughout the lifetime of the affected individual.3 Many patients face issues regarding identity, sexuality, and infertility, as well as possible cultural influences that may impact the patient’s reaction to the diagnosis or those of their family and friends.3 Thus, it is crucial that counseling and other forms of mental health support be provided to the patient.3
Pelvic Health Goals
A main goal for those with MRKH syndrome is gaining the ability to participate in penetrative sexual intercourse through the creation of a neovagina. First line of treatment to accomplish this involves self dilation.1 Self dilation techniques consist of progressive dilators being placed at the vaginal apex and inserted manually. Pelvic health physical therapists can help to assess patient readiness and educate the patient on how to perform self dilation.4 Another option is surgical intervention which consists of vaginoplasties using various grafts, and requires post surgical management of the neovagina to ensure it heals properly.1 One study looked into the quality of life and sexual function of those who had completed self dilation treatment vs. those who had undergone surgery.5 They found that scores for both quality of life and sexual function were about equal between groups.5 Therefore, both are great options that can provide desired results and satisfaction.5 Those with MRKH syndrome also have reproductive concerns. While both adoption and surrogacy have traditionally been the only options for MRKH sufferers, uterine transplant, albeit a newer procedure, is now a possibility.1,2 Although it is still considered experimental, it has been successful in the past in women with MRKH syndrome in allowing them to procreate.1,2
Questions or Concerns?
Our pelvic health physical therapists are here to help you with questions or concerns you have.
Written By:Anita K. Platis, SPT
References
- Herlin MK, Petersen MB, & Brännström M. Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome: a comprehensive update. Orphanet J Rare Dis. 2020;15(1):214. DOI:10.1186/s13023-020- 01491-9.
- Georgopapadakos N, Manoli A, Passia G, Skandalakis PN, Filippou D. Uterus Transplantation as a Therapy Method in Mayer-Rokitansky-Küster-Hauser Syndrome. Cureus. 2019;11(12):e6333. doi:10.7759/cureus.6333
- Bean EJ, Mazur T, Robinson AD. Mayer-Rokitansky-Kuster-Hauser syndrome: sexuality, psychological effects, and quality of life. J Pediatr Adolesc Gynecol. 2009;22(6):339–346.
- McVearry ME, Warner WB. Use of physical therapy to augment dilator treatment for vaginal agenesis. Female Pelvic Med Reconstr Surg. 2011 May;17(3):153-6. doi: 10.1097/SPV.0b013e31821bcd83.
- Kang J, Chen N, Song S, Zhang Y, Ma C, Ma Y, Zhu L. Sexual function and quality of life after the creation of a neovagina in women with Mayer-Rokitansky-Küster-Hauser syndrome: comparison of vaginal dilation and surgical procedures. Fertil Steril. 2020;113(5):1024-1031. doi: 10.1016/j.fertnstert.2020.01.017.