Pelvic Pain Awareness Month: Pudendal Neuralgia
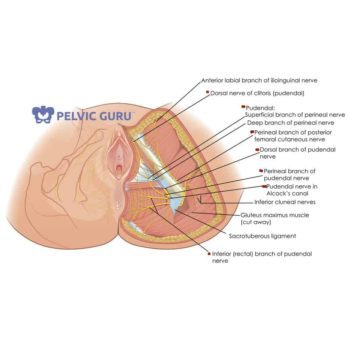
Anyone who has suffered from nerve compromise like sciatica or pudendal neuralgia knows how draining it can be on your life. Nerve pain is generally reported as sharp, shooting and/or burning pain along its distribution. Numbness is also commonly reported. The pudendal nerve can be compromised anywhere along its route from the sacrum to the anus, perineum, clitoris or penis. Individuals can often have bowel, bladder, and/or sexual dysfunction also. \
Causes
Pudendal neuralgia can occur after a traumatic event like a fall, childbirth, prolonged sitting or from surgery. When activities like biking, sitting in a car or prolonged sitting at work aggravate the pain it can be difficult to make the necessary lifestyle changes reducing pressure on the nerve and allowing it time to heal.
Compromise to the pudendal nerve causes nerve irritation, trigger points in surrounding muscles, tight connective tissue, and swelling. All these structures should be treated out to help ease symptoms.
Diagnosis
Diagnosis of pudendal neuralgia involves looking at the patient’s history and symptoms and ruling out serious medical conditions. Patients may undergo a MRN (Medical Resonance Neurography which is like a MRI for the nerves), EMG (Electromyography), or pudendal nerve motor latency test to assess the pudendal nerve itself.
Conservative Treatment
Conservative options to reduce pain include physical therapy and lifestyle changes. These lifestyle changes can include utilizing seat cushions or standing desks, avoiding bike riding, and avoiding deep squats. Another helpful lifestyle change includes dietary adjustments to avoid constipation. Wearing looser clothing may also help reduce symptoms.
Pelvic Health Physical Therapy
Pelvic health physical therapy can help to reduce the symptoms of pudendal neuralgia. Treatments can include internal pelvic floor trigger point release and myofascial release of the hip and low back to release tight muscles and connective tissue, which may be compressing the pudendal nerve. Manual therapy can also be used to help improve nerve mobility and blood supply to the nerve to facilitate healing. Relaxation exercises, postural education and breathing mechanics work in conjunction with manual therapy to decrease symptoms.
Call us at 212-233-9494 to speak to a physical therapist for more information or to schedule an appointment with a pelvic floor physical therapist.
Written by: Roseanne Cruz Schoen, DPT
Edited by: Keely Faridi, PT
References:
- Health Organization for Pudendal Education http://www.pudendalhope.info/node/9
- International Pelvic Pain Society www.pelvicpain.org