Perimenopause
Have you ever heard of perimenopause? If not, you are not alone. Often when women talk about menopause, they are actually referring to the period of time where the body prepares to stop ovulation, known as perimenopause.
Menopause is technically only one day in a women’s life cycle, where she has not had a period for exactly twelve months.
Perimenopause is when the trouble begins, as this transitional stage is where many women experience an array of symptoms as their hormones shift during the months or years leading up to menopause. Yes, you read that right, it can last up to 10 years.
It may happen sooner than you think
Some women start to notice changes in their mid-30s. However, most women arrive at menopause between the ages of 45 and 55, but perimenopause can begin a decade prior. And about 1% of women in the U.S. reach menopause at age 40 or younger.
How do I know if I have perimenopause?
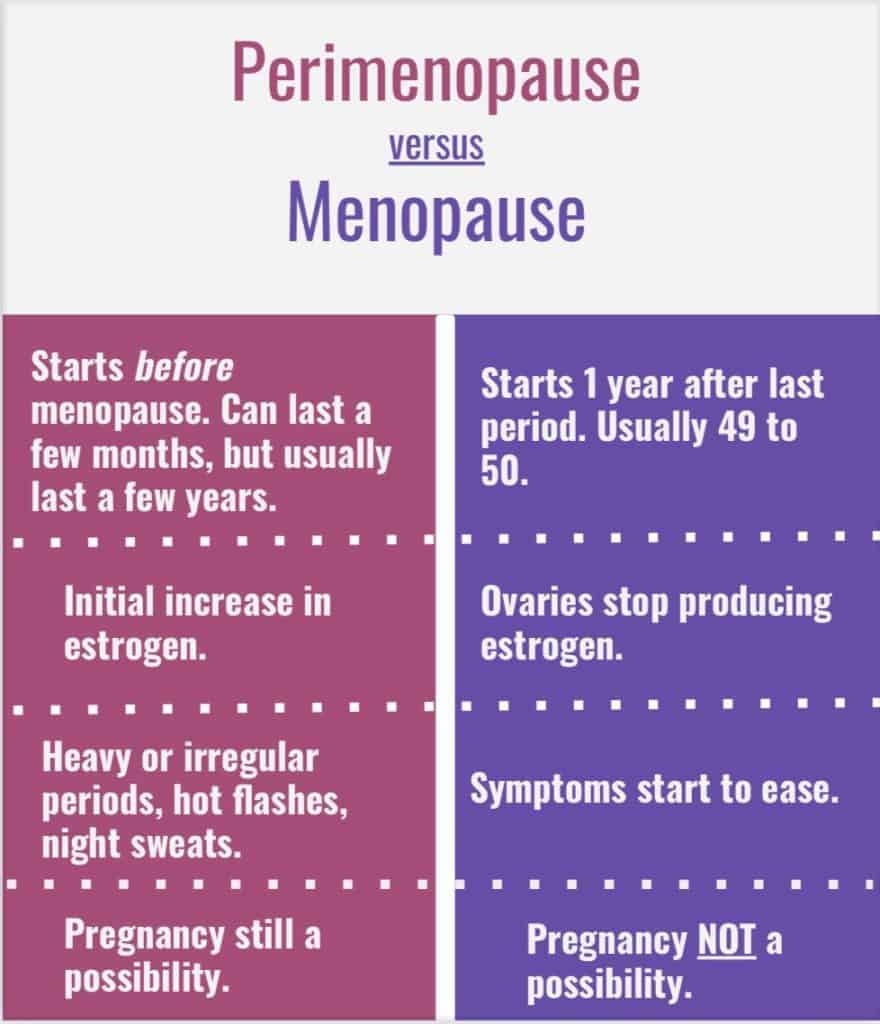
Perimenopause varies greatly from one woman to the next, but experts generally agree that it begins with irregular menstrual cycles. Bleeding may be heavy or light, and the length of the cycle variable, and may fluctuate from one month to the next. It is this irregularity that is indicative of perimenopause.
Erratic fluctuations of hormones during this stage make hormone or blood testing an unreliable diagnostic tool. The wide range of physical symptoms experienced by women are rooted in hormonal alterations, most notably circulating estrogen.
Know what to look for
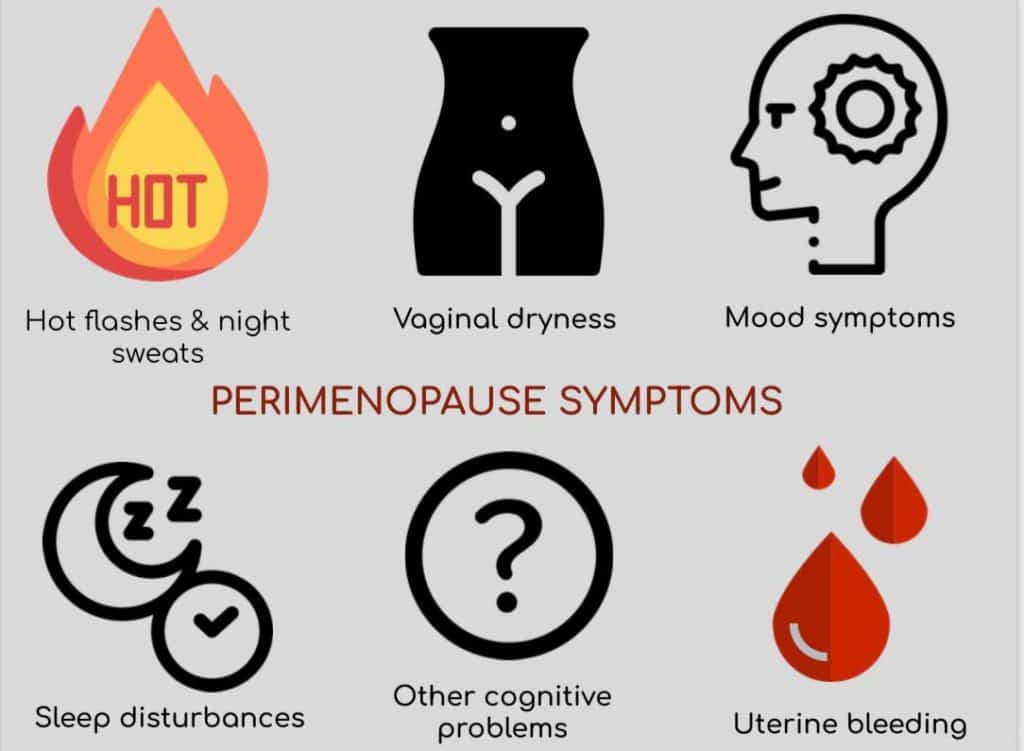
Perimenopause symptoms may be difficult for women and their providers to distinguish apart from common midlife events or changes due to aging. For example, many women experience hot flashes, but not all women, and some may mistake them for anxiety or stress.
Hot flashes and night sweats: An estimated 35%–50% of perimenopausal women suffer sudden waves of body heat with sweating and flushing that last 5–10 minutes, often at night as well as during the day.
Uterine bleeding: With less progesterone to regulate the growth of the endometrium, the uterine lining may become thicker before it’s shed, resulting in very heavy periods. Also, fibroids (benign tumors of the uterine wall) and endometriosis (the migration of endometrial tissue to other pelvic structures), both of which are fueled by estrogen, may become more troublesome.
Sleep disturbances: About 40% of perimenopausal women have sleep problems. Some studies have shown a relationship between night sweats and disrupted sleep; others have not. The problem is too complex to blame on hormones alone.
Mood symptoms: 10-20% of women experience mood symptoms during perimenopause. Some studies have linked estrogen to depression during the menopausal transition, but there’s no proof that depression in women at midlife reflects declining hormone levels. Some women may be more vulnerable than others to hormone-related mood changes. The best predictors of mood symptoms at midlife are life stress, poor overall health, and a history of depression.
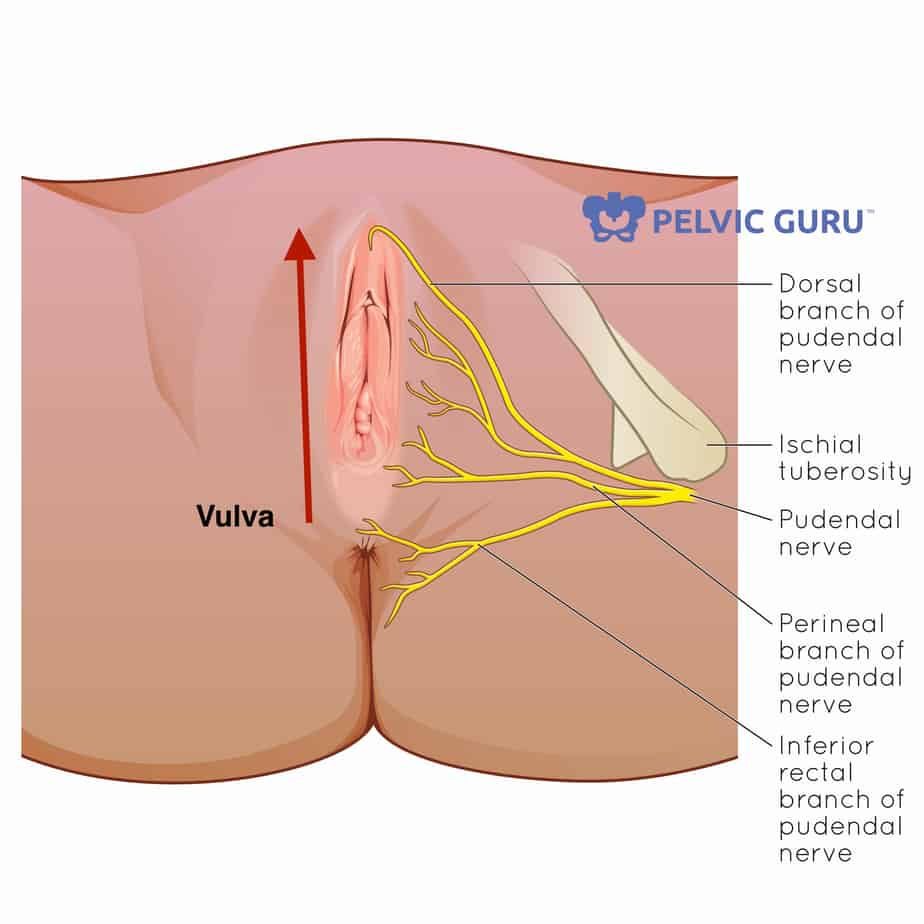
Vaginal dryness: Falling estrogen levels can cause vaginal tissue to become thinner and drier. Vaginal dryness (which usually becomes even worse after menopause) can cause itching and irritation. It may also be a source of pain during intercourse, contributing to a decline in sexual desire at midlife. Urinary tract infections may become more common as well.
Other problems: Many women complain of short-term memory problems and difficulty concentrating during the menopausal transition. Although estrogen and progesterone are players in maintaining brain function, there’s too little information to separate the effects of aging and psychosocial factors from those related to hormone changes.
Who can help?
Some women may only experience mild symptoms and never have cause for alarm. However, for others, symptoms may severely impact quality of life and should be addressed within a timely manner, to safely rule out other possible diagnosis. For optimal symptom management a multidisciplinary team of providers may be the best approach.
- Gynecologist or Urogynecologist
- Endocrinologist or Metabolic/Aging specialist
- Pelvic floor physical therapist
- Registered dietician
- Psychologist or psychiatrist
Empower yourself with knowledge
- The Massachusetts General Hospital Blum Center: https://www.massgeneral.org/blum-center/health-and-illness-resources/womens-health-pathfinder
- The National Women’s Health Information Center: https://www.womenshealth.gov/menopause
- The American College of Obstetricians and Gynecologists: https://www.acog.org/womens-health/faqs/perimenopausal-bleeding-and-bleeding-after-menopause
We can help!
Body Harmony Physical Therapy offers one-on-one treatment sessions and provides individualized treatment programs for each patient.
This blog was created for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a health condition or before beginning a new exercise routine.
Written By: Victoria Garrett, PT, DPT