The Journey Beyond Breast Cancer Surgery

There are many different surgical options for those with breast cancer or have ductus carcinoma in situ. (https://bodyharmonypt.com/breast-cancer-awareness-month/) Many times it comes down to an individual’s diagnosis. Early detection and intervention often leads to better short and long term outcomes.
So what happens after surgery? Can you jump right back into your life? Will you regain back the movement and strength in your body? Our blog this week goes through various things to look out for right after surgery and later on down the line.
Risks and Side Effects
There are some possible risks and side effects during or soon after surgery, which include:
- Problems with the anesthesia
- Bleeding
- Blood clots
- Fluid build-up in the breast or the donor site (for a tissue flap), with swelling and pain
- Infection at the surgery site(s)
- Infection can happen with any surgery, most often in the first couple of weeks after the operation. If you have an implant, it might have to be removed until the infection clears. A new implant can be put in later. If you have a tissue flap, surgery may be needed to clean the wound.
- Wound healing problems
- Fatigue
Long Term Considerations
Problems that can develop later on include:
- Tissue death of all or part of a tissue flap, skin, or fat
- Loss of or changes in nipple and breast sensation
- Problems at the donor site, such as loss of muscle strength, bulging of the abdominal wall, and dimples in the skin
- The need for more surgery to fix problems that come up
- Changes in the arm on the same side as the reconstructed breast
- Problems with a breast implant, such as movement, leakage, rupture, rippling of the skin over the implant, or scar tissue formation (capsular contracture)
- The most common problem with breast implants is capsular contracture. A scar (or capsule) can form around the soft implant. As it tightens, it can start to squeeze the implant, making the breast feel hard and look distorted. Capsular contracture can be treated. Sometimes surgery can remove the scar tissue, or the implant can be removed or replaced.
- Development of a rare type of cancer in the scar tissue around a breast implant
- Uneven breasts
The Healing Journey
Most individuals can start to get back to normal activities within 6 to 8 weeks. In general, healing will take time and patience.
- Sensation can be affected. Certain types of reconstruction surgery do not restore normal feeling to your breast, but in other types some feeling might return over time.
- It may take up to about 8 weeks for bruising and swelling to go away. Try to be patient as you wait to see the final result.
- It may take as long as 1 to 2 years for tissues to heal fully and scars to fade (the scars never go away completely).
- Talk with your surgeon about the type of bra to wear – sometimes it will depend on the type of surgery you had. After you heal, underwires and lace in your bra might feel uncomfortable if they press on scars or rub your skin.
- Call your doctor right away if you notice any new skin changes, swelling, lumps, pain, or fluid leaking from the breast, armpit, or flap donor site, or if you have other symptoms that concern you.
How Can PT Help Post-op Mastectomy/Reconstruction?
When the individual is medically stable and cleared, physical therapy can begin. Following surgery, individuals may experience a loss of strength or range of motion, or may also develop swelling, or lymphedema, if lymph nodes were also removed.
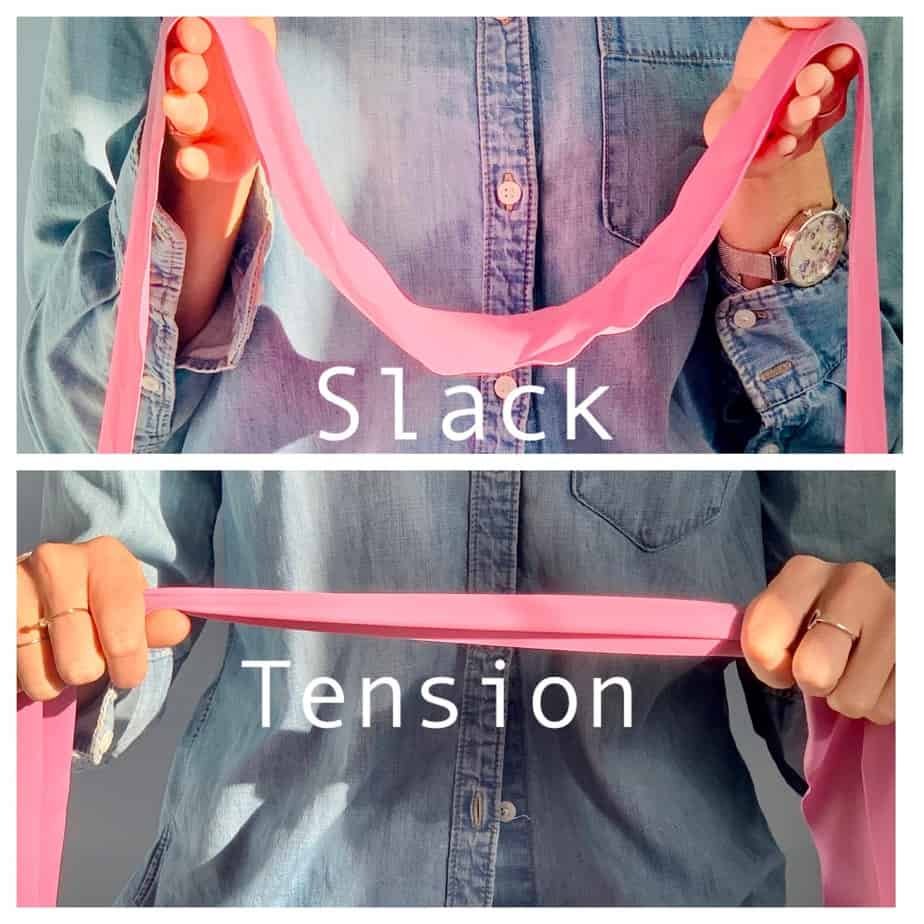
During the initial evaluation, the physical therapist will assess posture, range of motion and strength of the neck and arms, sensation, and look for any swelling of the arms or breast(s). If appropriate, manual lymphatic drainage and compression wrapping may be done to help reduce swelling.
On average, your physical therapist will see you between 1-3 times per week depending on how much help you need post-op. Our physical therapists see patients for an hour for each session and help you every step of the way as you make gains and meet your medical goals. They will provide you with an individualized home program. The aim of this is to continue making gains so the next time you’re in the office with us, we can keep you moving forwards, helping you gain more movement and strength. Our physical therapists will also educate you on how to care for yourself, watching for signs of lymphedema and give you the confidence to carry out appropriate skin care.
We are with you throughout your rehabilitation and available even after discharge for those random questions that come up. We have a lymphedema specialist in our downtown office. Reach out to our team of physical therapists at frontdesk@bodyharmonypt.com or call 212-233-9494.
LDT: https://bodyharmonypt.com/lymphedema-post-breast-cancer/