What is FGM/FGC? How does Physical Therapy play a part?

Last month one of our pelvic floor physical therapists Nazneen Vasi presented to Sahiyo on the role of pelvic health physical therapy and FGC/FGM. The full presentation is available to view here. We have added a click provided by Sahiyo below.
(Due to the personal and sensitive nature of this topic please be aware that some of the following information may be considered disturbing to some individuals, especially those that are continuing the journey in overcoming the psychological and physical consequences of the procedure. The information portrayed is intended to bring awareness to this procedure, educate and offer support.)
What is FGC/FGM?
FGM and FGC are used sometimes inter-changeably. FGC stands for female genital cutting while FGM is female genital mutilation. It is a procedure in which female genitals are removed for a non-medical reason. It’s usually performed in females under 18 and often without their consent. The severity of this procedure is varied and is classed Type I to Type IV.
- Type I consists of partial or total removal of the external clitoris and the clitoral hood.
- Type 4 which involves excision of the clitoris, labia minora, and labia majora, narrowing of the vaginal opening sometimes covering it entirely with the labia tissue, stitching the vaginal area closed and cauterization of tissues.
FGC is a less traumatizing term and more neutral, more often used by activists and local community groups. We will continue to use the term FGC for the remainder of the blog.
Below are illustrations of the 4 different types of FGC:
Where does FGC/FGM occur?
These procedures are performed for non-medical reasons and do not offer any health benefits. FGC predates Christianity and is thought to originate in East Africa. Many cultures continue to practice FGC to this day, with 200 million women and girls affected globally, in more than 90 countries. Many women continue to experience psychological and physical trauma from these procedures throughout their lives.
At what age does FGC/FGM occur?
It affects girls as young as newborns but more commonly is performed on girls under 15 and considered a rite of passage within a culture. In some cultures, adolescent girls agree to undergo FGC and it is accepted widely within the community. The issue of informed consent and fear of non-acceptance arises in these cases. Many times members of the family give consent for the girls to undergo the procedure and may even hold them down during it. Oftentimes, a traditional practitioner (not a medical doctor) performs these procedures and pain relief/anesthesia may not be offered.
Common Pelvic Health Symptoms
- Bleeding
- Chronic pain (ranging from mild to severe)
- Pudendal Neuralgia
- Difficulty passing urine
- Bacterial infections from the procedure
- Cyst, abscess or genital ulcer development
- Injury to genital tissue leading to pelvic pain or dyspareunia (pain with sex)
- Scar tissue formation
- Infection of reproductive system leading to infertility, menstrual issues
More involved procedures involve risk of severe blood loss, sepsis and death.
Long term effects of FGC/FGM
Many women report severe psychological trauma. This ranges from shame of their body and sexual emotions to avoidance of sexual experiences. Many women avoid sexual encounters and experience decreased sexual enjoyment as well as PTSD (post-traumatic stress disorder). In type III and type IV cases of FGC, sexual intercourse can only occur with re-opening of the vagina which is done surgically or through penetrative sexual intercourse. Sexual intercourse is frequently painful for weeks to months as the vaginal opening is recreated. Male partners may also experience pain during this process.
Many women who have undergone FGC experience more complications during childbirth. Old scar tissue may tear or has to be cut through. An episiotomy is generally performed to open the perineal area enough for the baby to be delivered. Some women are re-stitched after childbirth so the vaginal opening is smaller and/or tighter for their partners. This may cause further scar tissue to occur, thus leading to more pain, and the cycle continues.
FGC is illegal in many countries, however, it is still practiced at a community level. It was signed into federal law in 1996 in the US under the Female Genital Mutilation Act. It was deemed unconstitutional in 2018 and was passed at the state level in over 40 states. The federal law was amended and strengthened after a judge ruled it unconstitutional in 2018. The new federal law was signed in January 2021. Many families are able to get around this law and plan ‘vacation cutting’ trips abroad. Currently it is illegal to knowingly transport a girl outside the US to undergo FGC/FGM.
How does Pelvic Health Physical Therapy Play a Role?
Pelvic health physical therapists (PT) are uniquely placed in healthcare to address many issues women who have undergone FGC experience. A comprehensive pelvic evaluation will allow the PT to determine the best intervention available.
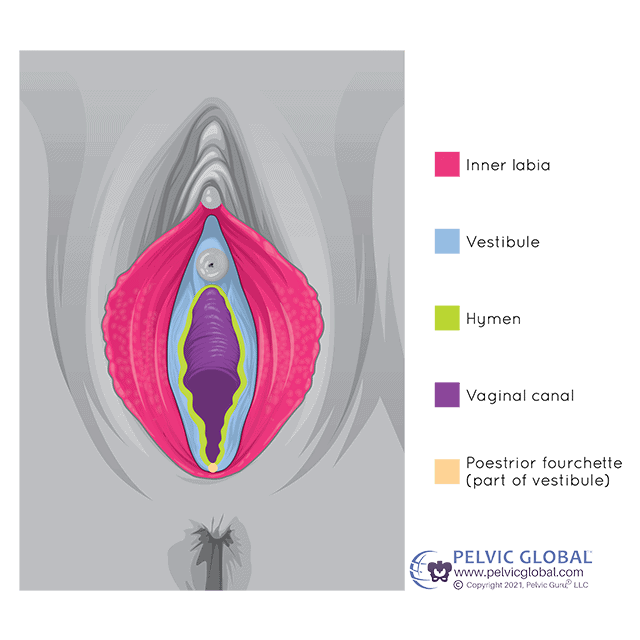
Treatments commonly include scar tissue manual therapy in which the scar tissue mobility is worked on. Mobile scar tissue reduces pain and tightness. Oftentimes scar tissue is adhered to other tissues (organs, muscles, fascia, nerves), and causes dysfunction within that tissue (menstrual cycle irregularities, muscle weakness, urinary dysfunction). Depending on the type of FGC performed any of the tissues below in the diagram may require soft tissue and scar tissue mobilization to improve flexibility, circulation and restore tissues to as close as possible to their former function.
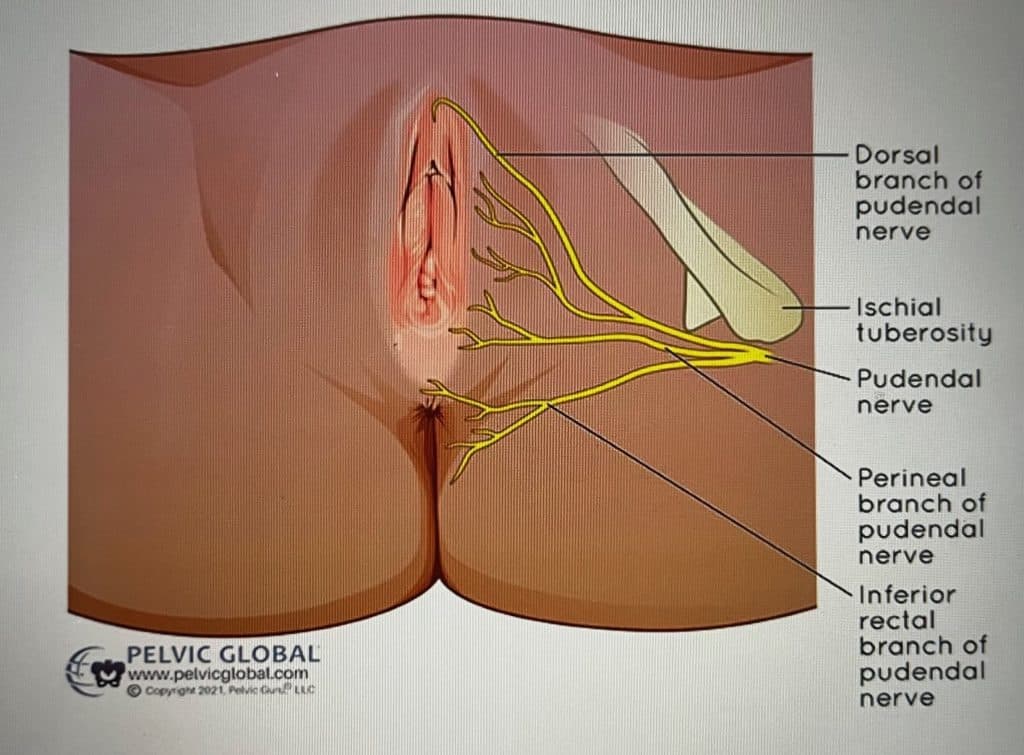
Other treatments include improving nerve mobility and function, particularly the pudendal nerve. The pudendal nerve attaches directly to the clitoris, vagina, labia and urethra. It supplies muscle control as well as sensation. It becomes injured directly through the trauma during the FGM procedure leading to pain and burning sensations. Pain is often worse in sitting, cycling, or tight fitting clothing (tights, jeans, etc). Pelvic floor physical therapists work directly on the nerve improving it’s mobility within the neural sheath and decreasing scar tissue which may entrap it.
Other PT Treatment Options
Other treatment interventions include specific stretching and strengthening for the pelvic floor muscles, re-alignment of the pelvis itself and re-education of the muscles to allow for better efficiency, functioning and pain relief. It’s important to note pelvic floor physical therapists are not psychologists, psychiatrists or talk therapists. We recognize the importance of having members of these interdisciplinary teams and highly recommend seeing one regularly. Often many, sometimes extreme, emotions come to surface when the physical tissues of the pelvic floor are worked on. It is really important to have the support network present in order to address deeper psychological concerns that may arise during sessions. Some women feel more comfortable bringing a member of their support team with them during a session who can be there before, after or sometimes during the session. We are sensitive specifically to the private nature of this specific pelvic health concern and work with patients to address issues appropriately.







