Posture for Easier Bowel Movements
No matter your background, lifestyle or career path pretty much everyone has something in common. We all poop.
Some indigenous cultures move their bowels while in a full squat. This is a similar position that toddlers naturally use, especially during the early potty training stages. Most moms who have gone through the potty training stage can attest to this.
What position makes it easier to go?
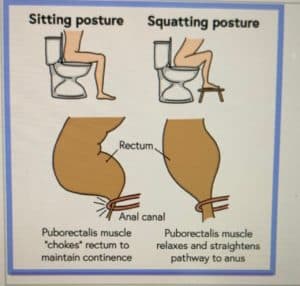
If we go back to the basics: pelvic floor muscles should be relaxed for stool to pass. This is easiest done when in a squat position. This position also coincidentally straightens the anorectal angle, which helps stool exit with less effort.
A full squat position can take its toll on the hips, knees, ankles, not to mention balance. The one thing this position has going for it is the pelvic floor muscles are relaxed in a full squat. Research shows there’s less effort when in a sitting position and the pelvic floor muscles are relaxed. A full squat position allows for the pelvic floor muscles to be in a relaxed state which reduces straining and the time it takes to have a bowel movement. This position also helps to straighten the anorectal angle. (More on this later)
There are several adjustments that can be made to mimic a full squat and doesn’t require so much effort or strain from the hips, knees and ankles.
Tips for Better Toileting Techniques
- Place a Squatty Potty ® under the feet. Alternatives include using a thickbook, or stack of books, a yoga block.
- Sit forwards over the knees or rest elbows on knees.
- Breath slow and deep. Inhale through the nose and exhale through the mouth.
- Use visualization techniques to help relax the body. Imagine the pelvic floor muscles opening as you inhale.
- Use pursed lip breathing. Imagine blowing into a straw or blowing up a balloon. Use this to help initiate the bowel movement.
- Avoid breath holding and straining. This may lead to hemorrhoids and muscle in coordination.
- Develop a routine. Go at the same time daily and train your body to become regular.
- Don’t sit on the toilet for more than 10 mins at a time when trying to move your bowels. If nothing happens after 10 mins, get up and try again a few hours later.

How is stool created? How does food and water make an impact?
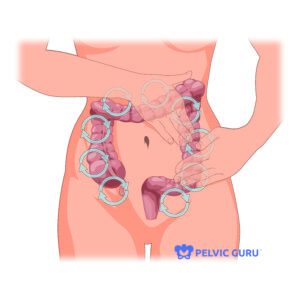
The food ingested collects in the stomach and is processed as it passes along the intestines. Nutrients, water, fats and sugars are removed along the way. The waste products are then pushed through peristalsis (rhythmical muscular movements) until they reach the large intestines where more water is removed. The end product collects within the rectum (the last 5-6 inches of the large intestine).
When enough waste product accumulates a small amount is allowed to enter the anal canal. The brain is able to determine if this is gas, liquid or solid. If the content is liquid we get an immediate alert to go to the bathroom as soon as possible (diarrhea). When it’s gas we can make the choice to pass it or not. If the content is solid we can also choose whether or not we want to go. Ignoring the sensation only works in the short term. Over time it leads to build up of more stool within the rectum over expanding the rectal tissues over time and reducing sensitivity.
As the rectum ends, it changes its course 90-110 degrees and turns into the anal canal. The anus, which is normally closed/contracted all the time (except for defecation) lies at the end of the anal canal. The puborectalis muscle (a pelvic floor muscle) slings around the anorectal angle helping to separate the two areas and keep you continent. During defecation the anorectal angle straightens to allow the stool to pass easier. Afterwards the anal sphincter closes and returns to its original state. A perfect bowel movement results in little wiping afterwards.
What other factors affect bowel movements?
The top three factors influencing bowel movements are diet, fluid intake and physical activity. Psychological factors also play a role. This includes conditions like depression or avoidance behaviors (unable to use a public bathroom). Age, pregnancy and the presence of pain can lead to more difficulty having a bowel movement.
Harder stools and conditions like constipation can make passing stool more challenging. There are several natural things you can do to improve constipation. Drinking hot liquids like hot water with lemon, tea or coffee can help stimulate bowel movements.
Alternatively methods include a bowel massage which stimulates the nerves of the large intestine and helps influence peristalsis. It takes about 5- 10 mins to perform.
Passing more firm or hard stools can be challenging and takes its toll on the body over time. The Bristol Stool Scale can be used to help you figure out if your diet needs a better balance of fiber and/or water. A normal stool is one that is Type 3 or 4 on the Bristol Stool Scale.
Too much water and too little fiber can lead to a stool being too loose or similar to diarrhea in consistency. Sometimes things like medication, muscle weakness or abnormality, and after childbirth due to injury/trauma to the pelvic floor can cause a loose stool.
Alternatively too little water and/or too much fiber leads to a harder more pellet like stool. This type of stool may take more time and effort to pass. It may also lead to hemorrhoids and pain.
How does pain affect bowel movements?
One other major factor in passing stool is the presence of pain. Pain is an inhibitor of muscles. This is especially true for the pelvic floor, which often becomes tightened and weaken as a result of being in a shorted position over long periods of time. In-coordination of muscles is termed dysynergy and is common with defecation. The muscles need to be taught how to coordinate properly and relax sufficiently for stool to be passed.
How does pelvic floor physical therapy help?
A pelvic floor physical therapist will perform a comprehensive evaluation looking at posture, strength, flexibility, neuromuscular control and muscle imbalances.
Physical therapy treatment options may include:
- myofascial manual therapy
- neuromuscular re-education
- visceral mobilization
- pelvic floor muscle relaxation and lengthening through trigger point release
- stretching and flexibility exercises
- relaxation exercises.
The internal rectal pelvic floor may also be evaluated. The pelvic floor muscles will be assessed for any tenderness, in-coordination, or weakness that may result in bowel dysfunction. Your physical therapist will also educate you on proper toileting techniques and diet, and review different stretches and self care techniques for your home program to improve bowel emptying.
Body Harmony Physical Therapy offers one on one physical therapy sessions for both pelvic floor and orthopedic conditions. Our treatments are for up to one hour in a private treatment room.
References:
- Consensus Statement of Definitions for Anorectal Physiology Testing and Pelvic Floor Terminology. https://fascrs.org/ascrs/media/files/downloads/Clinical%20Practice%20Guidelines/consensus_statement_of_definitions_for_anorectal-4.pdf
- Dyssynergic Defecation. https://iffgd.org/gi-disorders/dyssynergic-defecation/
- Comparison of straining during defecation in three positions: results and implications for human health. https://pubmed.ncbi.nlm.nih.gov/12870773/
- Bristol Stool Chart. https://www.bladderandbowel.org/wp-content/uploads/2018/03/BABC002_Bristol-Stool-Chart-Jan-2016.pdf
- Influence of body position and stool characteristics on defecation in humans. https://pubmed.ncbi.nlm.nih.gov/17026568/